Employers
Avoid the headaches associated with working with multiple vendors. Choose an industry leader and deliver the best benefits options to your employees for less.
Participants
The annual enrollment period is an important time of year. Take the opportunity to understand your benefits and compare available options. Your wallet will thank you.
Brokers
Let CPI manage your entire benefits lineup end-to-end. We’ll help you unlock economies of scale and give your clients bundled pricing they won’t find anywhere else.
Browse and shop the FSA Store.
Flexible Benefit
Administrative
Solutions
Easy-to-use benefits give members the tools and resources they need to spend smarter, save more, and invest in their healthcare. We provide the integrated solutions you need to simplify benefits and truly impact people’s lives. Work with an industry leader and deliver best practices at a lower cost.
COBRA
Consolidated Omnibus Budget Reconciliation Act
We will keep you up-to-date on the most recent changes in healthcare legislation.
HSA
Health Savings Account
We offer a paperless, digital way to manage your savings.
FSA
Flexible Spending Accounts
See how easy it is to spend and save like a pro.
HRA
Health Reimbursement Account
Reimbursable expenses like deductibles, copays, and more.
GALLAGHER
If that is what you need, contact CPI."
BABCOCK CONSULTING
ASSURED PARTNERS
Why Choose CPI?
Personal Service
Time is an invaluable asset for any business. With CPI as a partner, you’ll save more of it.
Secure Technology
We ensure all the safeguards are in place to protect your information in a digital world.
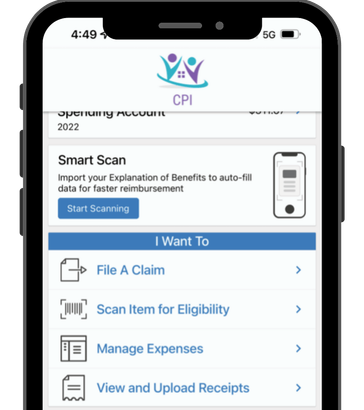
24 Hour Access
Access your benefits information 24/7 through our online resources and smartphone application.
Plan Compliance
Don't give a moment's thought to compliance. Our team of benefit experts has you covered.
QUICK LINKS
AUSTIN, TX
LAFAYETTE, LA
NEW ORLEANS, LA
We're here to help.
Customer Service Available
Monday-Friday: 7:30am–5pm, CST
© 2022 All Rights Reserved | CPI
Website by BlinkJar Media